Peri-acetabular Osteotomy (PAO)
Realigning the hip to preserve the natural joint and prevent arthritis.
Overview
PAO is a specialised procedure to correct hip dysplasia — a condition where the hip socket is too shallow or pointing in the wrong direction, leading to instability, pain, and if left untreated, early arthritis. The surgery involves carefully cutting and repositioning the pelvic bone to better support the femoral head. This preserves your native hip joint and may delay or prevent the need for a hip replacement.
Example of Periacetabular Osteotomy
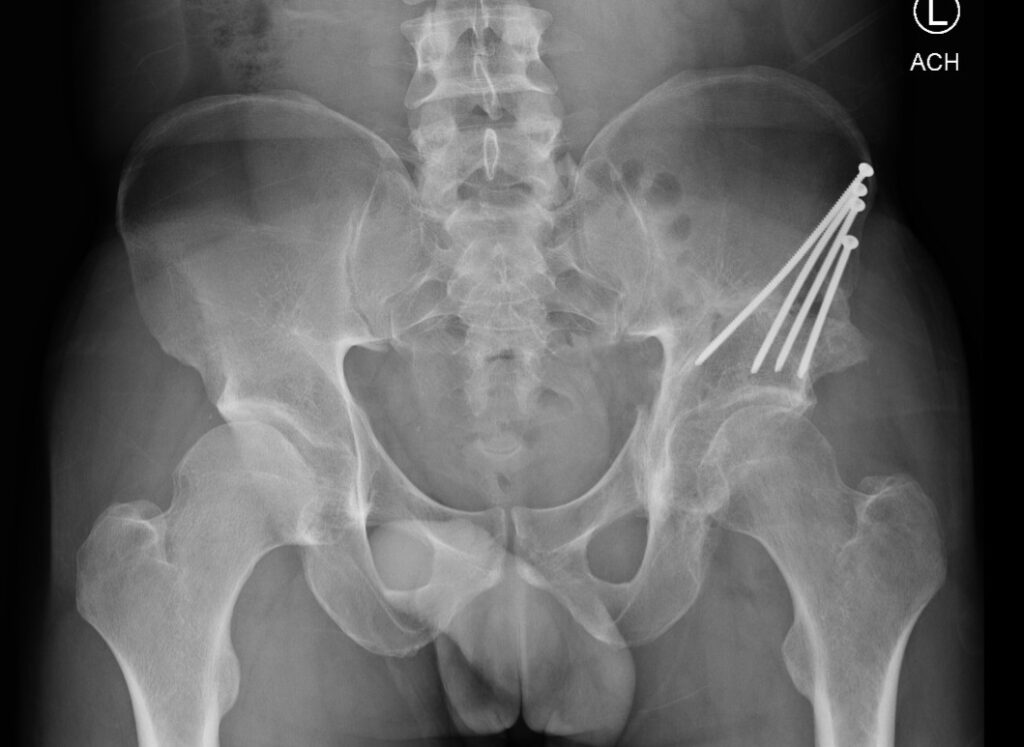
Postoperative xray of a partially healed periacetabular osteotomy
Indications
Surgical Approach
Risks
Periacetabular ostoetomy is a technically demanding procedure and is considered a "high risk" procedure by orthopaedic standards. However, these risks can be reduced with careful planning when undertaken by fellowship trained hip preservation surgeons.
Potential risks include:Significant bleeding or nerve injury (especially femoral or sciatic nerves)
Infection
Blood clots
Delayed bone healing
Over- or under-correction requiring revision
Ongoing pain, instability or progression to arthritis despite the procedure
We will go through your personal risk profile and ensure that every step is taken to minimise complications and maximise success.
Potential risks include:
We will go through your personal risk profile and ensure that every step is taken to minimise complications and maximise success.
Recovery Timeline
Peri-acetabular osteotomy is an involved procedure with extended post-operative recovery, however patient satisfaction is very high once the patient has fully recovered.
A typical recovery would be:
Hospital stay: 3–5 days
Crutches: ~6 weeks, then gradual weight bearing
Return to desk work: 6–8 weeks
Return to sport: 4–6 months
A typical recovery would be:
Frequently Asked Questions
Am I a good candidate for PAO?
You may be if you have hip dysplasia causing symptoms but your cartilage is still healthy. A thorough clinical and imaging assessment helps determine this. In people over the age of 40, or when the cartilage of the hip has begun to wear out, a total hip replacement or hip resurfacing may be more appropriate. Dr Robinson will discuss this with you in your consult.
What is the difference between a PAO and a hip replacement?
A PAO aims to preserve your natural hip and delay arthritis, making it ideal for younger patients. Hip replacement is generally for more advanced arthritis or older patients who are not in a position to undergo the more significant recovery that a PAO entails.
Are there any activity limitations after periacetabular osteotomy?
Once the ostoetomy has united, which is typically 6 months postoperative, there are no restrictions to your activity or lifestyle.
What happens if I wait too long before having surgery?
Unlike most conditions within orthopaedics, where patients are often advised to delay a surgery until there is a significant functional impairment, it is often advisable to undertake a PAO early in the patient's symptom journey. The earlier a PAO is done, the earlier the joint biomechanics are optimised, and the more likely it is that a potential hip replacement will not be required (or will be required later in life than it would have bee had the PAO not been peformed)
How painful is the recovery?
Some pain is expected initially, but this is managed with medications and regional anaesthesia. Pain generally improves significantly as the bone heals and mobility returns.
How likely is it that I will need a hip replacement later in life?
PAO is designed to preserve your natural hip and delay arthritis. Many patients avoid or postpone hip replacement, but outcomes depend on age, severity of dysplasia, and cartilage health.
Is pregnancy or childbirth affected by PAO?
Most patients can have children normally. PAO usually does not prevent vaginal delivery, but it’s important to tell your obstetrician about your surgery.
You may be if you have hip dysplasia causing symptoms but your cartilage is still healthy. A thorough clinical and imaging assessment helps determine this. In people over the age of 40, or when the cartilage of the hip has begun to wear out, a total hip replacement or hip resurfacing may be more appropriate. Dr Robinson will discuss this with you in your consult.
What is the difference between a PAO and a hip replacement?
A PAO aims to preserve your natural hip and delay arthritis, making it ideal for younger patients. Hip replacement is generally for more advanced arthritis or older patients who are not in a position to undergo the more significant recovery that a PAO entails.
Are there any activity limitations after periacetabular osteotomy?
Once the ostoetomy has united, which is typically 6 months postoperative, there are no restrictions to your activity or lifestyle.
What happens if I wait too long before having surgery?
Unlike most conditions within orthopaedics, where patients are often advised to delay a surgery until there is a significant functional impairment, it is often advisable to undertake a PAO early in the patient's symptom journey. The earlier a PAO is done, the earlier the joint biomechanics are optimised, and the more likely it is that a potential hip replacement will not be required (or will be required later in life than it would have bee had the PAO not been peformed)
How painful is the recovery?
Some pain is expected initially, but this is managed with medications and regional anaesthesia. Pain generally improves significantly as the bone heals and mobility returns.
How likely is it that I will need a hip replacement later in life?
PAO is designed to preserve your natural hip and delay arthritis. Many patients avoid or postpone hip replacement, but outcomes depend on age, severity of dysplasia, and cartilage health.
Is pregnancy or childbirth affected by PAO?
Most patients can have children normally. PAO usually does not prevent vaginal delivery, but it’s important to tell your obstetrician about your surgery.
Ready to Learn More?
If hip pain is holding you back, I’d be happy to meet with you to assess your symptoms, review your imaging, and discuss whether a periacetabular osteotomy is the right solution. Together, we’ll tailor a plan that suits your lifestyle, goals, and long-term joint health.
