Revision Hip Replacement
Restoring confidence and function. Supporting your future.
Overview
Revision hip replacement is a complex procedure performed when a previous hip replacement has stopped functioning well. Whether due to implant loosening, wear, infection, instability, or fracture, the goal of revision surgery is to restore mobility, relieve pain, and stabilise the joint using specialised implants and techniques.
This surgery often requires advanced planning, experienced surgical technique, and close post-operative care — all of which I provide as part of a carefully tailored approach for each individual patient, based on the reason for failure of their previous hip replacement and your goals.
This surgery often requires advanced planning, experienced surgical technique, and close post-operative care — all of which I provide as part of a carefully tailored approach for each individual patient, based on the reason for failure of their previous hip replacement and your goals.
Example of Revision Total Hip Replacement
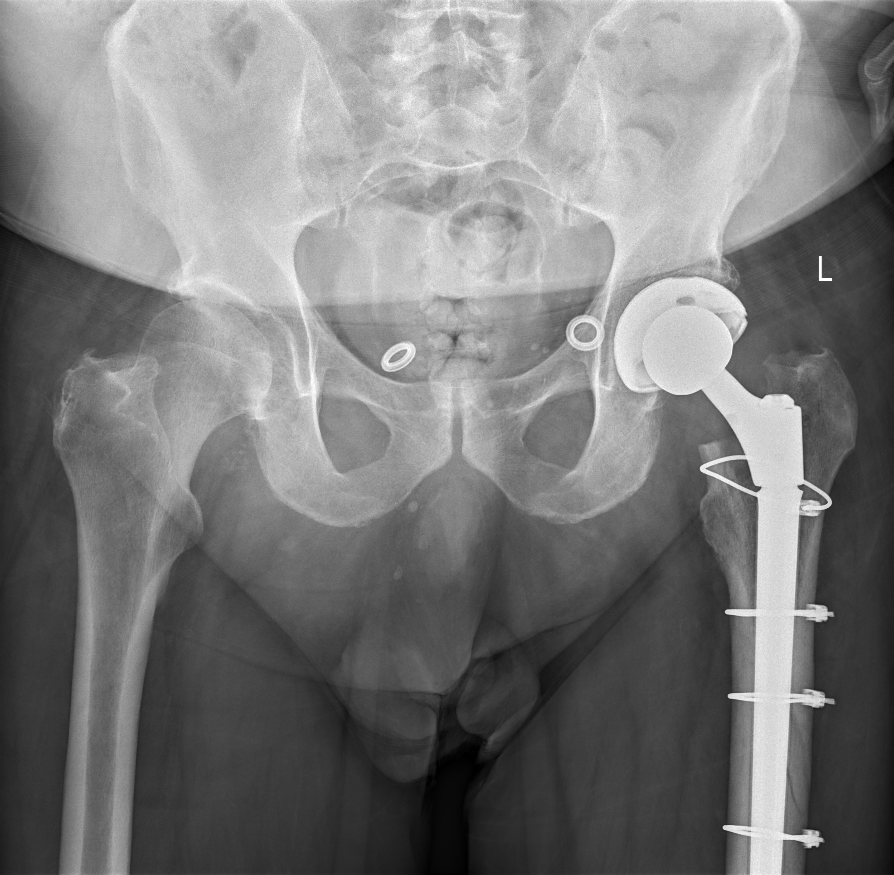
A revision total hip replacement, demonstrating cables to fix a femoral fracture
Indications
You may be a candidate for revision hip replacement if:
Your original hip replacement has loosened or worn out.
You have suffered from dislocations of your hip replacement
There is evidence of infection in or around the hip replacement
You have sustained a fracture either of the pelvis bone or femur (thigh bone) surrounding your hip replacement
You previous hip replacement has left you with a leg length discrepency or other inflammatory conditions. You have persistent pain or stiffness in your hip replacement
We assess each case with a combination of a detailed history, examination and investigations such as x-rays, advanced imaging, blood tests, and sometimes joint aspiration before discussing whether you would benefit from a revision of your hip replacement.
We assess each case with a combination of a detailed history, examination and investigations such as x-rays, advanced imaging, blood tests, and sometimes joint aspiration before discussing whether you would benefit from a revision of your hip replacement.
Surgical Approach
Revision surgery is more involved than primary hip replacement. It often requires:
Removal of old components (which may be loose, well-fixed, or broken)
Reconstruction of bone defects using bone grafts or augments
Insertion of revision-specific implants, which may be larger than standard to gain more grip in your pelvis or femur
Addressing soft tissue tension and stability to prevent future dislocations
The approach used (anterior or posterior) depends on the reason for failure of the previous hip replacement, type of implant and previous approach. Anterior approach revision surgery is preferred if possible, however more involved reconstructions are often more suited to the posterior approach.
The approach used (anterior or posterior) depends on the reason for failure of the previous hip replacement, type of implant and previous approach. Anterior approach revision surgery is preferred if possible, however more involved reconstructions are often more suited to the posterior approach.
Risks
Revision hip replacement carries a slightly higher risk profile than first time surgery:
Infection – more common, particularly in cases of previous infection
Dislocation– higher risk due to previously weakened soft tissues
Blood Loss– may be more likely in complex reconstructions
Nerve injury or numbness – still rare, but more likely due to scarring from previous surgery
Leg length discrepancy – minimised with careful peroperative planning
Fracture – possible during removal of previous components or insertion of revision components
Implant wear or loosening over time – less common with modern revision systems
We take every precaution to reduce these risks and provide long-term success.
We take every precaution to reduce these risks and provide long-term success.
Recovery Timeline
Recovery is typically slower than a primary hip replacement, but the goal remains the same — to regain reliable, pain-free mobility.
A typical Recovery would be:Hospital stay: 2-4 nights Walking with a frame or crutches: between 2-6 weeks, depending on the nature of the revision Return to driving: 2-6 weeks, depending on the approach and specific surgery requried Back to office work or light duties: 4-6 weeks Full recovery and return to gentle sport: 3-6 months, depending on complexity
Revision for infection may require a staged approach (temporary spacer, followed by second surgery), which involves longer rehabilitation.
A typical Recovery would be:
Revision for infection may require a staged approach (temporary spacer, followed by second surgery), which involves longer rehabilitation.
Frequently Asked Questions
What is the difference between a primary and revision hip replacement?
Primary hip replacement is the first-time surgery, while revision replaces or adjusts the existing components when they fail. Revision surgery is often more complex and requires longer recovery.
How do I know if my hip replacement has failed?
Persistent pain, instability, limp, leg length changes, or changes seen on X-rays or blood tests may indicate failure. Evaluation involves clinical examination and imaging.
Can a revision be done in one operation?
Yes, in most cases. However, if infection is present, a two-stage approach is often used — first removing the implant and treating the infection, then placing the new implant in a second surgery.
Are revision implants different?
Yes. They are often longer, modular, or augmented to compensate for bone loss and ensure stable fixation.
Will recovery be harder than the first hip replacement?
It can be more involved, but with experienced care, most patients regain excellent function. You may need more physiotherapy and a longer period of walking aids.
Is the outcome as good as a first hip replacement?
While not always identical to a primary replacement, outcomes are still excellent in most patients, with significant pain relief and functional improvement.
Primary hip replacement is the first-time surgery, while revision replaces or adjusts the existing components when they fail. Revision surgery is often more complex and requires longer recovery.
How do I know if my hip replacement has failed?
Persistent pain, instability, limp, leg length changes, or changes seen on X-rays or blood tests may indicate failure. Evaluation involves clinical examination and imaging.
Can a revision be done in one operation?
Yes, in most cases. However, if infection is present, a two-stage approach is often used — first removing the implant and treating the infection, then placing the new implant in a second surgery.
Are revision implants different?
Yes. They are often longer, modular, or augmented to compensate for bone loss and ensure stable fixation.
Will recovery be harder than the first hip replacement?
It can be more involved, but with experienced care, most patients regain excellent function. You may need more physiotherapy and a longer period of walking aids.
Is the outcome as good as a first hip replacement?
While not always identical to a primary replacement, outcomes are still excellent in most patients, with significant pain relief and functional improvement.
Ready to Learn More?
If hip pain is holding you back, I’d be happy to meet with you to assess your symptoms, review your imaging, and discuss whether a hip replacement is the right solution. Together, we’ll tailor a plan that suits your lifestyle, goals, and long-term joint health.
